What is COPD
Chronic Obstructive Pulmonary Disease is the name given to the progressive narrowing of the airways. This narrowing may result from an obstruction of the airways in patients with Chronic Bronchitis or Emphysema.
1. What is Emphysema?
Emphysema is brought about by cigarette smoking which results in chemical changes that destroy lung tissue which reduces elasticity and the airways tend to close.
2. What is Bronchitis ?
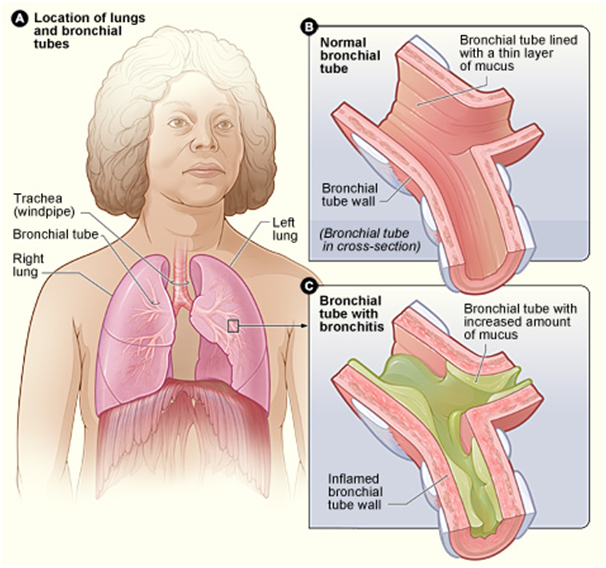
Bronchitis is a condition in which the bronchial tubes become inflamed. These tubes carry air to your lungs.
People who have bronchitis often have a cough that brings up mucus. Mucus is a slimy substance made by the lining of the bronchial tubes. Bronchitis also may cause wheezing (a whistling or squeaky sound when you breathe), chest pain or discomfort, a low fever, and shortness of breath.
Figure “A” shows the location of the lungs and bronchial tubes in the body. Figure “B” is an enlarged, detailed view of a normal bronchial tube. Figure “C” is an enlarged, detailed view of a bronchial tube with bronchitis. The tube is inflamed and contains more mucus than usual.
The two main types of bronchitis are acute (short term) and chronic (ongoing).
Symptoms
Dyspnea: It is basically when a person becomes short of breath. It is a subjective experience of breathing discomfort that consists of qualitatively distinct sensations that vary in intensity. People with COPD, most commonly emphysema or bronchitis, frequently have chronic shortness of breath and a chronic productive cough.
Wheezing:sWheezing is a sign that a person may be having breathing problems. The sound of wheezing is most obvious when breathing out(exhaling), but may be heard when taking a breath too(inhaling). There are various causes for wheezing, like asthma, bronchitis, emphysema/COPD, heart failure, pneumonia, smoking, etc.
Fatigue: Fatigue is a state of awareness describing a range of afflictions, usually associated with physical and/or mental weakness. Physical fatigue is the inability to continue functioning at the level of one’s normal abilities.
Cough and Morning Headache are general symptoms.
Diagnosing COPD
COPD may be diagnosed by checking the medical history of a patient. To check for family history with regard to tobacco, exacerbations and basic symptoms.
A chest X-Ray
Spirometry: assessment of severity
Arterial Blood Gases measurement to detect chronic respiratory failure.
Treatment for COPD
Medications: Bronchodilators are medicines that usually come in the form of an inhaler. They work to relax the muscles around your airways help open them and make it easier to breathe. Inhaled steroids help prevent the airways from getting inflamed.
Pulmonary Rehabilitation:Your doctor may recommend that you participate in pulmonary rehabilitation or ‘rehab’. This is a program that helps you learn to exercise and manage your disease with physical activity and counselling. It can help you stay active and carry out your daily tasks.
Physical Activity Training:Your doctor or a pulmonary therapist recommended by your doctor might teach you some activities to help your arms and legs get stronger and/or breathing exercises that strengthen the muscles needed for breathing.
Lifestyle Changes:Lifestyle changes such as quitting smoking can help you manage the effects of COPD.
Oxygen Treatment: If your COPD is severe, your doctor might suggest oxygen therapy to help with shortness of breath. you might need oxygen all of the time or just some of the time-your doctor will work with you to learn which treatment will be most helpful.
Surgery: COPD patients with very severe symptoms may have a hard time breathing all the time. In some cases, doctors may suggest lung surgery to improve breathing and help lessen some of the most severe symptoms.
Managing Complications: Symptoms of COPD can get worse all of a sudden. When this happens, it is much harder to catch your breath. You might also have chest tightness, more coughing or a change in your cough and a fever.
Measuring Oxygen Levels
Oxygen levels are measure in two different ways, namely ABG(Arterial Blood Gas) and Pulse Oximetry.
Arterial Blood Gas: An Arterial Blood Gas is a blood test that is performed using blood from an artery. It involves puncturing an artery with a thin needle and syringe and drawing a small volume of blood. The test is used to determine the pH of the blood, the partial pressure of carbon dioxide and oxygen, and the bicarbonate level.
Pulse Oximetry: Pulse Oximetry is a non-invasive method allowing the monitoring of the saturation of a patient’s haemoglobin. A sensor is placed on a thin part of the patient’s body, usually a fingertip or earlobe, or in the case of an infant, across a foot. Light of two different wavelengths is passed through the patient to a photodetector. The changing absorbance at each of the wavelengths is measured, allowing determination of the absorbance due to the pulsing arterial blood alone, excluding venous blood, skin, bone, muscle, fat, and nail polish.
Oxygen Therapy for COPD
Long Term Oxygen Therapy is usually given over a minimum of 15 hours a day, including overnight when arterial hypoxaemia worsens during sleep. There are several ways to deliver oxygen:
Oxygen Concentrators
Oxygen Gas Cylinders
Liquid Oxygen Devices
O2 Therapy & After
Long term oxygen treatment may improve your quality of life. It can help a patient live longer even with severe COPD and low oxygen levels. The patient may notice less shortness of breath and have more energy.
Why Oxygen
LTOT is used for COPD if you have low levels of oxygen in your blood. It is used mostly to slow or prevent right-sided heart failure. Oxygen can also be used at home if the oxygen level in your blood is too low for long periods. Regular use can reduce the risk of death from low oxygen levels.
Does O2 therapy work
Studies show that using oxygen at home for more than 15 hours a day increases quality of life and helps people live longer when they have severe COPD and low blood levels of oxygen. Using oxygen may also improve confusion and memory problems. It may improve impaired kidney function caused by low oxygen levels.
Risks
Generally there are no risks from oxygen treatment as long as you follow your doctor’s instructions. But oxygen is a fire hazard, so it is important to follow safety rules. Do not use oxygen around lit cigarettes, open flames, or anything flammable.
Exercise/Sleep/Air Travel
Exercise: For some people with COPD, blood oxygen levels drop only when they exercise or are very active. Using oxygen during exercise may help boost performance and reduce shortness of breath for some people.
Sleep: During sleep, breathing naturally slows down because the body doesn’t need as much oxygen. Sleep related breathing disorders are quite common in people with COPD, and many will have significantly low blood oxygen levels during sleep.
Air Travel: The level of oxygen in airplanes is about the same as the oxygen level at an elevation of 8000ft. This drop in oxygen can really affect people with COPD. If you normally use oxygen or have borderline-low oxygen levels in your blood, you may need oxygen when you fly. Traveling with oxygen is usually possible. But it is important to plan ahead before you travel.